We often hear people coin the phrase whiplash or complain of having whiplash when their neck is sore but how much do you really know about this common issue so many people seem to suffer with?
The first cases of whiplash related injuries were first reported back around 1919 and was originally known as “railway spine” following its connection to rail collisions. It is now the widely known, non-medical term used to describe the neck pain following soft tissue injuries of the neck, specifically the ligaments, tendons and muscles. Contrary to popular belief, you cannot just get whiplash from car accidents. Although they are the most common cause of whiplash, many people can experience this injury following a fall; after a concert or festival involving a lot of head banging and for all those dare devils out there, after a bungee jump.
What actually happens?
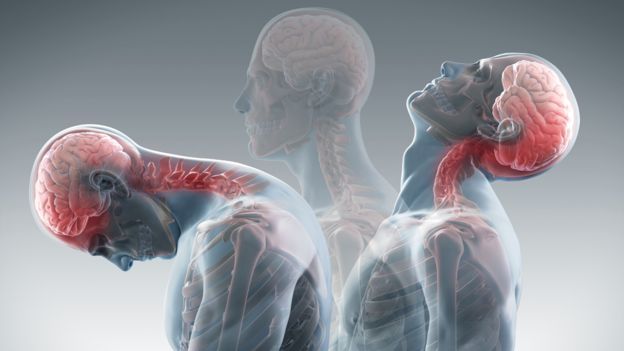
Whiplash is caused by sudden acceleration/ deceleration disturbance of the neck. For instance, during a car accident where the patient’s vehicle is hit from behind, this can be broken down into 4 stages
1. Initial; the neck is in a stable position with normal cervical lordosis present.
2. Retraction; As the seat is pushed forward due to impact, the cervical spine is forced to retract causing an ‘S’ shape in the cervical region. During this phase injuries will occur in the lower cervical vertebrae.
3. Extension; The neck is forced into full extension causing damage to the soft tissue of the anterior neck.
4. Rebound; the most dangerous phase. As the seatbelt supports the trunk, the head goes into full flexion which causes damage to the posterior tissue of the neck.
Symptoms
The Quebec Task Force (QTF) coined what is known as WAD or Whiplash Associated Disorders in 1995, which cover a range of common symptoms experienced and reported by patients with a whiplash injury. These include:
Aches and pain in the neck and back; referral pain through the shoulders; headaches and sensory disturbances such as pins and needles in the arms and/ or legs.
Symptoms can vary from experiencing mild pain for a few days to severe disability. Surprising, 50% of people with a WAD will report symptoms 1+year following the initial injury.
Diagnosis
Following an accident or when your neck isn’t feeling quite right after an accident or injury involving velocity or quick acceleration/deceleration of the head, a trip to your local GP is the next port of call.
Diagnostics involved include taking a history, a thorough head and neck exam, x-ray to diagnose a fracture if present and perhaps further medical imaging to determine other injuires.
From here, the grade of whiplash associated disorder may be determined.
Yes, the QTF also divided the WAD’s into 5 categories to determine the severity of the whiplash. These are:
0- Nil pain experienced or physical signs observed
1- Pain and or stiffness of the neck, tenderness however no physical signs observed.
2- Complaints of pain or stiffness in the neck, decreased range of movement and tenderness under touch
3- As grade 2 plus neurological signs such as sensory deficits, decreased deep tendon reflexes and weakness.
4- Fracture or dislocation and or spinal cord injury.
90% of most whiplash claims are a Grade 1 and 2.
What to do after diagnosis
So you have been diagnosed with a whiplash injury and luckily fall in with the 90% who have a Grade 1 or 2 WAD, you’re in luck and have come to the right place.
Recent research recommends early intervention following diagnosis and physical therapy and active therapy which enhances pain reduction and also shortens post-injury disability. Active physical therapy should be considered the treatment of choice in patients with QTF grade 1-2 whiplash.
Active therapy includes soft tissue, trigger point therapy, joint mobility of the cervical spine, posture, coordination and stability training and electrotherapy such as TENS.
So, what are you waiting for? If you have been in an accident or feel that you are experiencing these symptoms which may be a result of a whiplash injury, see your GP or pop in for a chat with your physical therapist for further examination and treatment options.
Danielle Guy
Occupational Therapist